What is a High Tibial Osteotomy?
High tibial (proximal tibial) osteotomies are surgical procedures designed to correct leg alignment issues. These operations can transform a bow-legged individual, bringing their alignment back to normal or even slightly knock-kneed. The process involves creating a controlled surgical fracture in the upper part of the tibia, often on the inside, effectively 'cracking' the bone. However, a 10-15 mm hinge of bone on the outer side of the tibia is left intact. This 'opening wedge' allows for the adjustment of leg alignment. To secure this correction, a plate and screws are used, and bone graft material is placed in the created wedge for support.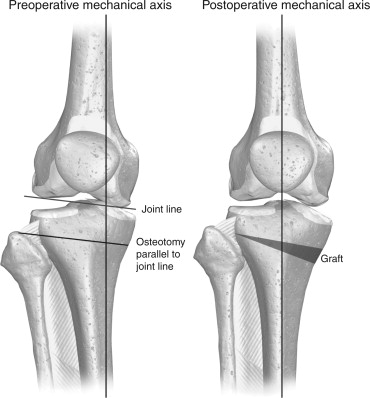
Do I Need a High Tibial Osteotomy?
High tibial osteotomies serve various important indications, and they can significantly improve the quality of life for patients with specific knee issues.
Arthritis on the Inside of the Knee: The most common indication is for patients who develop arthritis on the inner side of their knee, often due to a prior partial medial meniscectomy. These individuals are typically bow-legged, but the rest of their knee cartilage is relatively healthy. In such cases, a proximal tibial osteotomy can shift the weight-bearing load to the center or outside of the knee, effectively alleviating arthritis symptoms. It can also delay the need for a partial or total knee replacement. For younger patients, especially those under 50, this procedure is highly preferred as it allows them to continue high-level and high-impact activities without the concerns associated with artificial knee components.
Preparing for Meniscus Transplants and Cartilage Resurfacing: Another common indication is in patients who are bow-legged and require a medial meniscus transplant or a medial compartment cartilage resurfacing procedure. When such procedures are performed on the inside part of the knee in bow-legged patients, the risk of failure is considerably higher. Therefore, a proximal tibial osteotomy, either performed concurrently or prior to these treatments, is recommended to improve their chances of success.
Ligament Problems: Patients with chronic posterolateral corner injuries who are bow-legged face a high risk of graft stretching on the outside of their knee. In such cases, a proximal tibial osteotomy is often suggested either before or along with lateral collateral ligament and posterolateral corner reconstruction to enhance stability.
Other less common indications include patients with:
Cruciate Ligament Reconstructions: These patients may have a tibial tilt, typically backward, which can jeopardize the success of an anterior cruciate ligament (ACL) graft. A closing wedge osteotomy can help alleviate this issue and increase the chances of a successful ACL reconstruction.
OtherFlat Tibial Slope and Chronic PCL Tear: For patients with a flat tibial slope and chronic posterior cruciate ligament (PCL) tears, particularly those with medial compartment arthritis, increasing the slope by tilting the tibia backward can effectively enhance stability in PCL-deficient knees. This procedure may eliminate the need for later PCL reconstruction in some cases.
These diverse indications for high tibial osteotomies demonstrate the versatility of this surgical approach in addressing various knee conditions and improving patients' overall knee health and functionality.
Does Bow-Legged Require Surgery?
For patients with osteoarthritis in the inner part of their knee, especially those who are bow-legged, the utilization of a medial compartment unloader brace can be a valuable preliminary assessment tool. It helps determine whether a proximal tibial osteotomy would be a suitable course of action. Based on our clinical experience, we strongly recommend the use of a medial compartment unloader brace in such cases. We have found these braces to be remarkably effective in identifying patients who are likely to benefit from a proximal tibial osteotomy.
This approach not only provides valuable insights into the potential success of the surgery but also allows for a more personalized and informed decision-making process, ultimately leading to better outcomes for patients dealing with knee osteoarthritis and alignment issues.
How Successful is a Proximal Tibial Osteotomy?
The results of proximal tibial osteotomies in delaying the necessity for a total knee arthroplasty are quite promising. Studies indicate that approximately 75% to 80% of patients still experience relief from knee pain at the 10-year mark, with some remarkable reports suggesting that even up to 20 years post-surgery, 65% of patients continue to enjoy a life free of knee discomfort.
The key advantage of opting for tibial reshaping over a partial or total knee replacement arthroplasty is the ability to maintain an active lifestyle. Individuals can continue participating in higher-level activities like climbing, hiking, tennis, and jogging, without the constant worry of their prosthetic joint wearing out. However, it's important to exercise caution when considering high-impact activities, such as long-distance running, as there is a potential risk of earlier knee wear due to the proximal tibial osteotomy surgical procedure.
This approach not only extends the lifespan of the knee but also enhances the quality of life for patients who wish to remain active and engaged in various physical pursuits. It underscores the significance of making informed decisions that align with both individual goals and the long-term health of the knee joint.
What is the Recovery After High Tibial Osteotomy?
In the postoperative phase following a high tibial osteotomy, patients typically undergo a period of partial to non-weightbearing for the initial 8 weeks. X-rays are performed at this juncture to assess the progress of osteotomy healing, serving as a critical factor in deciding when weightbearing can be safely initiated. The gradual return to weightbearing usually starts at one-quarter of the body weight per week, continuing until the 3-month mark when new x-rays are taken. If these x-rays reveal sufficient healing, patients can begin to wean off crutches once they can walk without a limp.
One notable aspect of high tibial osteotomy recovery is its relative rapidity during this phase. Unlike situations where ligament healing or other complexities are involved, patients can focus on a progressive quadriceps strengthening program using stationary bikes and elliptical machines. This proactive approach enables individuals to return to their daily activities sooner.
Our experience indicates that most patients achieve their maximum level of improvement about six months postoperatively, provided that strength is adequately restored. This level of improvement tends to persist for at least 5-7 years after surgery, if not longer. This underscores the potential for a sustained and improved quality of life for individuals who choose the high tibial osteotomy procedure to address their knee concerns.
