Patella Dislocation
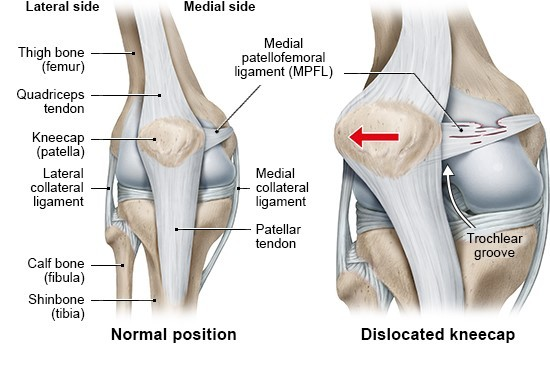
Patients who have a tracking problem in the patellofemoral joint - the patella does not stay in the groove on the femur - are vulnerable to a spectrum of conditions. These include subluxations, in which the patella slips partially but not completely comes out of the trochlea, as well as dislocations, a traumatic injury in which soft tissues are damaged as the patella completely “jumps” the track and then comes forcibly back into place. Because the bone always dislocates outward, the ligament on the inside - the medial patellofemoral ligament (MPFL) tears or stretches.
People who experience a first-time patella dislocation frequently do so while participating in sports, causing the knee to suddenly buckle and they fall. “Because ACL tears often happen in the same way, and because they are much more common than patella dislocations, it is important to rule out an ACL tear.
Physical signs of dislocation include significant swelling of the knee and an “apprehension sign”, an anxious response to the orthopedist’s translating the patella outward and attempting to mimic the dislocation. An MRI after kneecap dislocation reveals damage to the ligament, bruises on the bone inside of the patella and on the outside of the femur that occur when the kneecap “re-locates” back in place. The MRI is also helpful in evaluating the knee for evidence of cartilage injury which is very common after dislocations.
Risk Factors for Dislocation
Subluxation and Dislocation Risk Factors
Subluxation and dislocation risk factors can affect a specific demographic, primarily young women with hypermobility, and athletes who may encounter more traumatic dislocations during sports activities. While subluxation and dislocations can occur in men and boys, it's less common. Individuals within these groups tend to share common anatomical variations recognized as risk factors. These include: Shallow or Absent Groove on the Trochlea or Femur: When the groove (track) that guides the patella is shallow or absent, it results in less control over the patella's movement within the joint, making it easier to dislocate.
Abnormal Patellar Tendon Insertion on the Tibia (Knock Knees): People with an unusual insertion of the patellar tendon on the tibia (shin) with knock-kneed posture are at greater risk. This condition exerts a force on the patella, pulling it outward from the trochlear groove.
High-Riding Kneecap: A patella located higher up on the femur than normal increases the risk of dislocation. It has to travel a longer distance during knee flexion before engaging fully in the groove, making the joint vulnerable to instability during this phase.
Dr. Amit Meena emphasizes that despite the intense pain experienced during a dislocation, patients may feel little to no pain in between instability episodes. Unfortunately, this can lead to delayed treatment, even though cartilage damage continues to progress with each subluxation or dislocation.
Pain and Symptoms : Pain is often found at the lower and outer margins of the kneecap, beneath the patella and on the outside of the knee. However, some patients may experience more widespread pain throughout the joint, particularly when there's severe inflammation. This uneven distribution of stress underneath the kneecap causes pain, which can be due to abnormal patellar tilt or muscle weakness.
Patellofemoral pain and related issues occur more frequently in women than in men. Women typically have a more valgus or knock-kneed stance, which naturally pulls the patella toward the outside of the leg and increases the risk of uneven stress distribution.
Contributing Factors : Muscle tightness and soft tissue problems, such as tight hamstrings and the iliotibial (IT) band, can also contribute to these issues. Conversely, women with hypermobile, loose soft tissues can develop patellofemoral pain due to muscle weakness and the inability of supporting muscles to balance or unload the patella, causing lateral displacement.
Evaluation and Treatment : Orthopedic surgeons and sports medicine specialists evaluate patellofemoral pain with a thorough physical examination, assessing imbalances from the feet to the hips. Additional factors that may exacerbate pain include flat feet, hip rotation abnormalities, IT band tightness, and hip flexor issues. MRI and x-ray images are often used to assess bone structure, alignment, and cartilage surfaces of the kneecap and trochlea.
Treatment Approach : The standard of care for first-time dislocations is non-operative, allowing torn ligaments to heal naturally. However, an MRI is crucial to evaluate the extent of damage even after one dislocation. Surgery is necessary if a piece of bone or cartilage is dislodged, as these loose bodies can lead to pain and discomfort if left untreated.
In cases not requiring surgery, the knee is typically immobilized in a splint or brace for a brief period to reduce swelling and pain. Physical therapy is the primary treatment after the first dislocation, helping restore normal range of motion and strength. This therapy can continue for 2-3 months, with some athletes taking up to 4-5 months to return to their pre-injury level of play.
After experiencing a patella or knee cap dislocation, individuals face an increased risk of it recurring, either as subluxation or full dislocation. Statistics show that the risk of recurrence after the first dislocation is between 20-40%, and it rises to over 50% after the second dislocation. Younger patients under 25, especially those with open growth plates, can face re-dislocation rates of up to 70%.
Surgery is recommended for individuals with more than one dislocation to stabilize the knee cap and protect the cartilage underneath, preventing arthritis in young patients. Cartilage damage can occur during instability events, with MRI showing damage in over 70% of cases.
Recovery from knee stabilization surgery typically takes 6-9 months, involving extensive physical therapy and activity modification.
For patients with cartilage defects, current cartilage repair techniques can be more beneficial than for those with generalized osteoarthritis. Traumatic events like dislocations often result in isolated cartilage damage, and repairing these defects with cartilage from other parts of the knee can be effective.
Stabilizing the knee before cartilage damage occurs or worsens is essential, as knee stabilization procedures offer predictable good results and long-term protection for cartilage and joint health.
Why Choose KNEECARES – The Superspeciality knee Clinic for your Patella Dislocation
At KNEECARES, our team of experts boasts extensive experience in addressing kneecap pain. Our approach centers on conservative treatments as the first line of defense, reserving surgery as a last resort.
We believe in exhausting non-surgical options to manage and alleviate kneecap pain before contemplating surgical interventions. Only when these conservative treatments prove ineffective in providing relief and restoring normal function do we consider recommending surgery. Our primary goal is to improve the well-being of our patients, ensuring that they regain mobility and enjoy life without the burden of kneecap pain and limitations.
