Total Knee Replacement
Total knee replacement (TKR), also known as total knee arthroplasty, stands as one of the remarkable success stories in the field of orthopedic medicine. The reason behind its success lies in the remarkable pain relief and the restoration of function that patients often experience post-surgery. Thanks to advancements in implant designs and refined surgical techniques, the majority of TKR patients can anticipate enjoying well-functioning knee joints for a considerable period, typically spanning 15 to 20 years, encompassing more than 85% to 90% of individuals.
However, it's essential to acknowledge that like any medical procedure or implanted device, there may be instances where TKR procedures or implants face challenges and may not endure indefinitely. In such cases, patients may find themselves at a juncture where knee revision surgery becomes a necessary consideration.
What are the different types of knee replacement surgery?
Two primary categories of knee replacement procedures exist:-
Knee anatomy
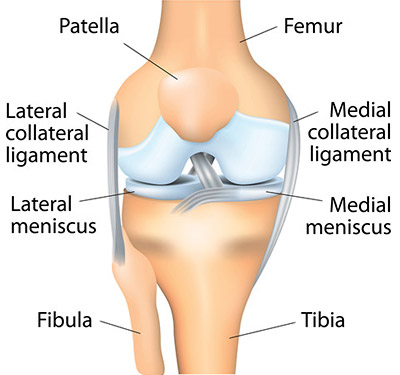
To comprehend the concept of a total knee replacement, also referred to as total condylar total knee arthroplasty, it's essential to have a grasp of the knee's intricate structure. The knee is a complex joint comprising three major bones:-
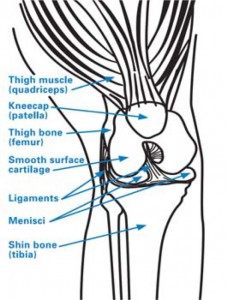
Within the knee joint, robust ligaments connect the powerful thigh and calf muscles to these bones, facilitating precise control over knee motion and function. Moreover, the joint is cushioned by cartilage, including structures like the meniscus, and other soft tissues that envelop the bones, ensuring smooth gliding motion.
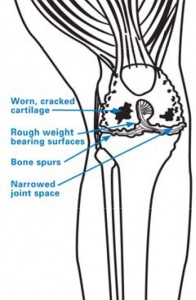
During knee flexion and extension, the end of the femur articulates with the end of the tibia, while the patella smoothly moves in front of the femur. However, when the protective cartilage that cushions the joint deteriorates or is entirely worn down, the bones start to rub against each other, resulting in rough and abrasive surfaces. This degeneration leads to the development of Knee Osteoarthritis treatment, marked by pain and stiffness, which severely hampers everyday movements such as walking. In the context of knee replacement surgery, the artificial implants are meticulously designed to replicate the smooth surfaces of a healthy knee, thus restoring function and alleviating pain.
When you bend or straighten your knee, the end of the femur rolls against the end of the tibia, and the patella glides in front of the femur. When the cartilage that cushions the joint degrades or is worn away completely, the bones rub together and become scraped and rough. This causes inflammation known as osteoarthritis, which results in pain and stiffness that make walking and other movements difficult. The implants used in knee replacement are smooth like the surfaces of a healthy knee.
How is a total knee replacement performed?
The surgical procedure begins with a carefully placed incision in the knee, followed by the gentle repositioning of the patella (kneecap) to provide access to the joint. If any bone spurs are detected, often associated with osteoarthritis, they are meticulously removed to create a smoother surface.
The subsequent steps involve the removal of the menisci positioned between the femur and tibia, along with the anterior cruciate ligament (ACL). In certain cases, the posterior cruciate ligament (PCL) may also be addressed, although it may be retained in some knee replacement types.
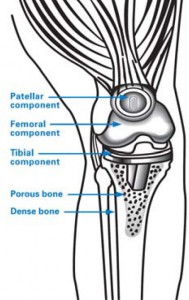
During the primary phase of the operation, we meticulously trim and extract cartilage and portions of bone from the upper tibia and the lower femur. The femur's removed segments are known as femoral condyles, which are then replaced with metal implants to establish new joint surfaces. These implants are strategically designed to mimic the original anatomy, ensuring optimal functionality. If the kneecap has also undergone deterioration, its underside may be addressed, typically replaced with a polyethylene implant.
Subsequently, the various layers of tissue are skillfully repaired using dissolvable sutures, and the skin incision is securely closed with sutures or surgical staples. A protective bandage is carefully applied around the knee, and the patient is gently transported to the recovery area.
This advanced approach to knee restoration results in a significant improvement in joint function, providing patients with the opportunity to regain an active and pain-free lifestyle.
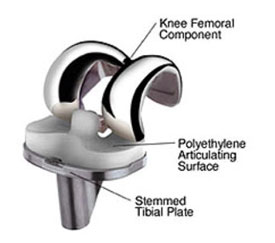
Fixed-bearing knee implant with a polyethylene articulating surface (plastic tray) sandwiched between the metal tibial implant and metal femoral implant.

Side-view illustration of a knee with a fixed-bearing knee implant in place.

X-ray of a knee after total knee replacement, showing the implanted prosthesiS
What are knee replacement implants made of?
The choice of knee replacement prosthesis design and materials is a highly personalized decision, tailored to each patient's unique needs. The key components of the implant primarily consist of metals, often titanium or chrome-cobalt alloys. These implants are securely affixed in place through either a cement bonding agent or osseointegration, where a porous metal stem extends into the tibia, allowing the patient's natural bone to integrate with it seamlessly.
Between the tibial and femoral implant surfaces, a crucial plastic platform or spacer, typically made of polyethylene, is meticulously inserted to facilitate smooth joint movement.
Femoral components are predominantly composed of metal alloys, such as cobalt chromium, or metal-ceramic alloys featuring oxidized zirconium. The patellar component, on the other hand, is crafted from plastic, specifically polyethylene. Meanwhile, the tibial insert component shares the same material – polyethylene. The tibial tray component offers versatility in material selection, with options including:
This personalized approach to prosthetic selection ensures that each patient receives the most suitable implant materials and design, setting the stage for a successful and durable knee replacement procedure.
Can I avoid or postpone a knee replacement?
The decision to undergo surgery for knee joint arthritis hinges on several critical factors, carefully evaluated in each patient's unique situation. These factors include:-
Each patient's specific condition and lifestyle are taken into account to determine the most suitable treatment plan, whether surgical or non-surgical, ensuring optimal care for arthritis-related knee issues.
How do I know if I need knee replacement surgery?
When these symptoms and circumstances align, it's crucial to explore surgical interventions as a potential solution to address the underlying knee issues and restore functionality and comfort.
How long does a knee replacement last?
Knee replacement implants are designed to provide functionality for an extended period, typically ranging from 15 to 20 years in approximately 85% to 90% of patients. However, it's essential to recognize that these implants have a finite lifespan, and they may eventually require attention.
After this 15 to 20-year timeframe, the natural wear and tear that occurs with daily use can potentially lead to implant loosening. Depending on the individual patient, this may manifest with various symptoms, including:-
When any of these symptoms arise, the recommendation may be knee Revision or total knee replacement surgery to replace the original implant. It's particularly critical to address infections promptly, as they pose a unique challenge. While infections following knee replacement surgery are rare, the implant itself cannot defend against infection if harmful bacteria are introduced into the body. Swift action is necessary to ensure the best possible outcome in such cases.
How long does knee replacement surgery take?
A total knee replacement procedure typically lasts between 60 to 90 minutes, although the entire duration of your time in the operating room may extend to over two hours. The thoroughness and precision of the surgery ensure comprehensive attention to detail, allowing for a successful and effective knee replacement experience.
How long is it before I can walk after a knee replacement?
Following surgery, patients typically advance from the use of a straight cane, walker, or crutches within a short period, often as soon as two or three days after the procedure. With each passing day, the distance and frequency of walking will gradually increase, promoting a smooth recovery process. Many individuals find that they can resume driving a car within three to six weeks after surgery, and they can generally return to most of their regular activities within or before six weeks. While full recuperation and the restoration of full strength and mobility may take around four months or longer, it's not uncommon for patients to experience significantly improved mobility just one month after their knee replacement surgery.
Knee replacement recovery time and recuperation
Rehabilitation, or physical therapy, is an integral part of your recovery journey and typically begins within 24 hours of your surgery. Our dedicated nursing staff will ensure your comfort and mobility, assisting you with gentle movements and repositioning until you can independently move around.
Shortly after your surgery, a skilled physical therapist will visit your room to guide you through appropriate exercises and monitor your progress. These exercises focus on improving your range of motion, which not only helps prevent circulation issues but also strengthens your muscles. Your personalized rehabilitation program will commence once you are medically stable, and your doctor provides the necessary orders to initiate postoperative mobility.
Your active participation and motivation during physical therapy are crucial for the success of your surgery and overall recovery. The physical therapist will work with you to achieve various milestones, including sitting at the bedside with your feet on the floor, safely transferring in and out of bed, walking with the assistance of mobility aids (walker, cane, or crutches), and even mastering the art of climbing stairs with the aid of appropriate devices. Your progress will be carefully monitored and guided to help you regain your mobility and independence.
What can I expect at KNEECARES - The Superspeciality Knee Clinic?
KNEECARES leads the way in cutting-edge knee replacement procedures. Our commitment to patient satisfaction is reflected in our top rankings, and we pride ourselves on achieving the lowest infection rates in the country for knee replacements.
Our dedication to research and advancement drives us to continually improve our methods and outcomes. This includes innovations such as smaller incisions, the use of new implant materials and designs, and the integration of sophisticated instrumentation into our procedures.
At KNEECARES, we consistently adopt the latest surgical techniques and employ state-of-the-art technology to ensure that our patients receive the Best knee replacement in Jaipur with possible care and the most Advanced knee replacement treatments available. Your well-being and successful outcomes are our primary goals.
