PCL Reconstruction
If you are experiencing pain in the ligament behind the knee, you may be a candidate for PCL knee surgery.
The posterior cruciate ligament, often referred to as the PCL, stands as the most robust ligament within the knee joint. Regrettably, a torn PCL is frequently overlooked and remains undiagnosed.
The primary role of the posterior cruciate ligament is to prevent the backward translation of the knee, particularly at higher knee flexion angles. Consequently, individuals often experience issues related to deceleration, navigating stairs or inclines, and participating in activities that involve twisting, turning, or pivoting.
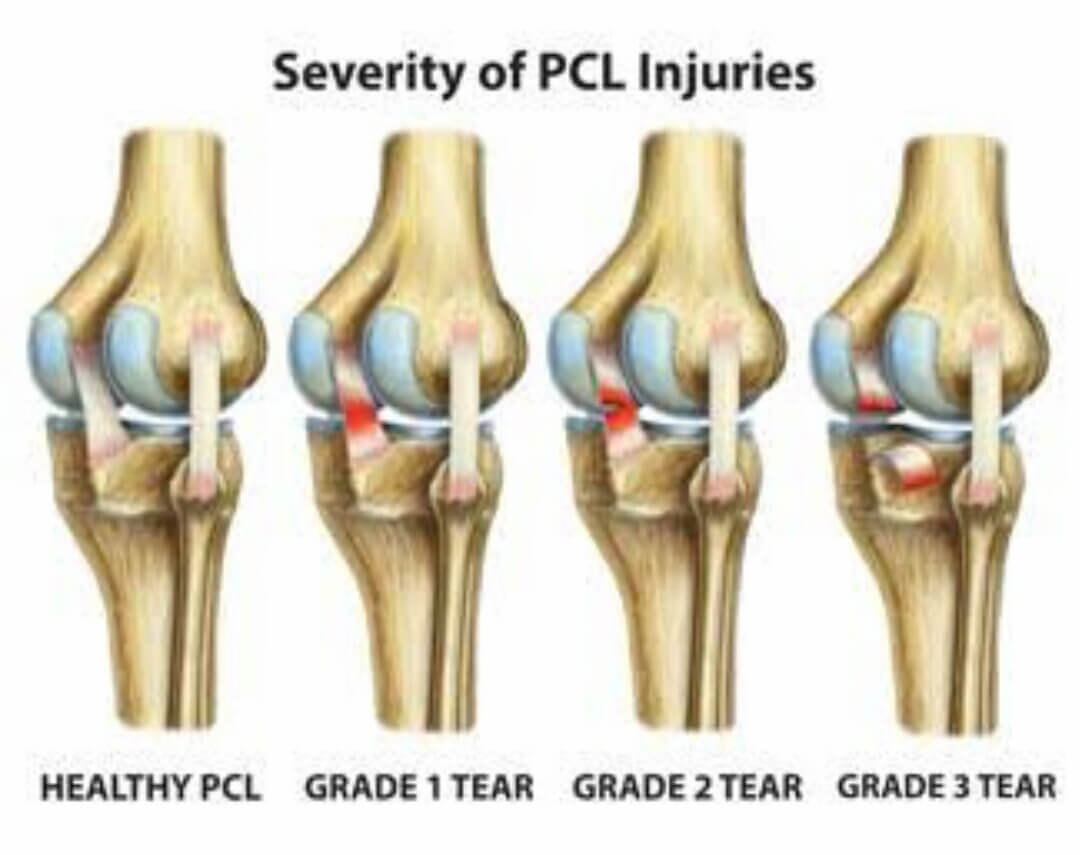
PCL injuries are typically classified based on the extent of damage to this critical ligament:
Understanding the severity of a PCL injury is crucial for appropriate treatment and management. Whether it's a partial tear or a complete rupture, addressing PCL injuries effectively is essential for restoring knee function and mobility.

When to Have PCL Surgery
Determining the right timing for PCL surgery is a critical decision. Generally, Dr. Amit will recommend PCL surgery for injuries categorized as grade 3 PCL tears. However, for high-level athletes, opting for PCL reconstruction sooner is often advisable. This is because the outcomes of acute reconstructions tend to be far more favorable compared to chronic reconstructions.
In cases where PCL surgery is deemed necessary, Dr. Amit conducts a comprehensive assessment of the patient to identify any potential concurrent injuries. Astonishingly, in our experience, about 90% of patients with symptomatic PCL tears that significantly impact their functionality also have associated injuries, such as posterolateral corner injuries or posteromedial injuries. Consequently, isolated PCL reconstructions make up only around 10% of the total PCL reconstructions that we perform. This underscores the importance of a thorough evaluation to address all pertinent issues when planning PCL surgery.
When to Have PCL Surgery
Dr. Amit Meena typically recommends PCL surgery for injuries classified as grade 3. However, for athletes performing at a higher level, opting for PCL reconstruction sooner is often advisable due to the considerably superior outcomes associated with acute reconstructions, as opposed to chronic ones.
In cases where PCL surgery is deemed necessary, Dr Amit Meena conducts a comprehensive patient assessment to identify potential concurrent injuries. Remarkably, in our experience, nearly 90% of patients with symptomatic PCL tears that significantly limit their functionality also have additional injuries, such as posterolateral corner or posteromedial injuries. Consequently, isolated PCL reconstructions constitute only around 10% of the total PCL reconstructions that we perform. This underscores the importance of a thorough evaluation to address all relevant issues when planning PCL surgery.
Double-Bundle PCL Reconstruction
For our surgical PCL reconstructions, we employ a technique known as double bundle reconstruction using allografts. This approach is favored due to historical data indicating less-than-ideal outcomes with single bundle reconstructions in the literature. Our goal is to continually improve surgical techniques to enhance patient outcomes and provide the best care possible.
PCL Reconstruction Success Rate
Our experience shows that PCL reconstruction is highly successful in restoring knee stability for our patients. This success is not only evident in objective measures, such as improved PCL stress x-rays, but also in the subjective evaluations of our patients, who consistently report positive outcome scores. We're dedicated to delivering the best results and ensuring the well-being of our patients.PCL Rehab Program
Our PCL rehabilitation program is designed to optimize the recovery process. Starting as early as day one, patients can engage in prone knee flexion at a range of 0-90°. We strongly recommend the continuous use of a PCL Rebound brace for six months following the surgery, with the exception of showering or changing clothes. This approach helps reduce posterior gravitational stress on the knee. For high-level athletes, we advise wearing a PCL Rebound brace at least through the first competitive season after PCL reconstruction to provide additional protection and unload the PCL graft while it remodels.
While some may view our rehabilitation program as aggressive, we're proud to report that none of our grafts have stretched out over time. Instead, our approach has led to a faster recovery of knee motion, a reduced risk of knee stiffness, and an overall higher level of function. We're committed to delivering top-notch care and helping our patients regain their quality of life.
How long does it take to recover from a sprained PCL? How long does it take to recover from a PCL tear?
The recovery time for a PCL tear varies based on the severity of the injury. For minor sprains, classified as grade 1 PCL tears, athletes might return to competition in as little as 2 or 3 weeks. This typically requires the knee swelling to subside, strength to recover, and the athlete's endurance and agility to return to normal. In the case of grade 2 PCL tears, which involve more knee instability, recovery without surgery may take up to 6 weeks. Dynamic PCL braces like the PCL Rebound brace can help maintain knee stability during this healing process.
For grade 3 PCL tears, which result in significant posterior tibial translation due to the PCL tear, there's a growing consensus on the effectiveness of PCL reconstruction surgery. While dynamic PCL braces can assist in maintaining knee stability, it's crucial to recognize that patient-reported outcomes are much better when surgery is performed within the first few weeks after the injury rather than waiting for 6 weeks or longer. In cases of grade 3 PCL tears with instability, surgical reconstruction is recommended. These surgeries typically require 9-12 months for complete healing and recovery. We're dedicated to providing the best care and helping our patients get back to their active lifestyles as swiftly and safely as possible.
Can a PCL injury heal on its own?
While the PCL differs from the ACL surgery in its ability to heal, it's essential to understand that some natural healing can take place thanks to the synovial membrane surrounding the PCL. However, gravity can be detrimental to the healing process in these cases. Therefore, when dealing with a significant PCL tear, it's advisable to consider options like a cast or a dynamic PCL brace. These measures help hold the knee in a reduced position, increasing the likelihood of the PCL healing in a tighter, more stable position. This can significantly improve the chances of a successful recovery and restored knee function.
How successful is PCL surgery?
The success rates for PCL reconstruction are quite promising, with most studies reporting a successful reconstruction in 85-90% of cases. This means that the vast majority of individuals who undergo PCL reconstruction can expect a positive outcome and a significant improvement in knee stability and function.
When to have PCL surgery?
Currently, the general recommendation is that individuals, especially athletes, who experience a grade 3 PCL tear should seriously consider PCL reconstruction. For those with grade 2 PCL tears, it's advisable to think about reconstruction if they face challenges with activities that involve deceleration, descending inclines or hills, or if they start to develop pain in the kneecap joint or along the inside of their knee. It's important to note that medium to long-term PCL tears can potentially lead to issues like patellofemoral and medial compartment arthritis, so any pain in these areas should be carefully monitored.
In many cases, the severity of a PCL tear can be assessed through PCL stress x-rays, which measure the degree of posterior tibial translation (backward movement of the shinbone) on the injured knee compared to the unaffected knee. Typically, if the stress x-rays show an increase of more than 8 mm in posterior tibial translation in the injured knee, surgery should be considered. If the increase is less than 8 mm, it may indicate that the patient is guarding against the injury or that there is a partial PCL tear. In such situations, it's recommended to start with a rehabilitation program, followed by a re-evaluation, including repeat x-rays, after a few weeks to confirm the PCL's condition. This approach helps determine the appropriate course of treatment based on the patient's progress.
What is PCL reconstruction recovery time?
Recovering from a PCL reconstruction is different from an ACL reconstruction due to the PCL's larger size and the use of a bigger graft during the procedure. This means that the PCL requires more biologic healing time. In most PCL rehabilitation programs, there is an initial 6-week period of non-weightbearing, during which a dynamic PCL brace is utilized. Following this phase, a program spanning up to 6 months postoperatively is designed, during which patients or athletes are advised to avoid activities such as running, twisting, turning, and pivoting.
At the 6-month mark, if PCL stress x-rays show good healing of the PCL reconstruction, patients can gradually begin a jogging program and engage in side-to-side activities, provided they have regained sufficient quadriceps strength and do not experience valgus collapse (inward collapse of the knee) during activities like single-leg squats. Our experience, particularly with professional and Olympic athletes, has shown that they can often return to full competition between 9 and 12 months after surgery. However, the exact timeline for recovery is contingent on whether the patient has undergone an isolated PCL reconstruction or if there are other concurrent ligament injuries that require attention.
What is a PCL reconstruction protocol?
Rehabilitation following a PCL reconstruction is not a one-size-fits-all approach; it needs to be tailored to the patient's specific injury. Typically, the initial six weeks post-PCL reconstruction involve a non-weightbearing phase, during which patients perform motion exercises while lying on their stomach, focusing on prone knee flexion. This approach mitigates the impact of gravity and aids in PCL healing without the concern of developing stiffness in the knee.
At the six-week mark, patients begin weightbearing exercises and gradually wean off crutches once they can walk without a pronounced limp. During this phase, they primarily engage in straight-ahead (single-plane) activities up until the six-month point. They are encouraged to work on a stationary bike and progress to using an elliptical machine to strengthen their quadriceps muscles. However, it's crucial to allow the graft to heal sufficiently before moving on to higher-level activities to prevent the PCL graft from stretching over time.
Throughout the first six months post-surgery, patients wear a dynamic PCL brace to counteract the effects of gravity and safeguard the graft from stretching. Our experience has shown that this approach significantly enhances the outcomes of PCL reconstructions, making it an essential part of the rehabilitation process.
Is a PCL reconstruction necessary?
The posterior cruciate ligament, or PCL, is, without a doubt, the knee's powerhouse when it comes to ligaments. A complete PCL tear can unleash havoc in the knee, leading to excessive motion and making activities like descending hills, stairs, or inclines a real challenge. Scientific studies back up the notion that patients grappling with chronic PCL tears in these circumstances often find themselves contending with arthritis within a span of 5 to 7 years. Consequently, when patients face significant knee instability due to PCL damage, the prevailing recommendation is to opt for a PCL reconstruction.
It's crucial to acknowledge that historically, PCL reconstructions fell short of the stellar success rates enjoyed by ACL reconstructions. This disappointment even led many surgeons to abandon PCL reconstructions when they discovered that the outcomes weren't any better than what the patients started with. However, in the modern era of medicine, marked by anatomic-based techniques, especially the double-bundle PCL reconstruction, things have taken a turn for the better. These advanced approaches have not only enhanced PCL reconstruction outcomes but also earned validation in scientific literature, placing them on par with the achievements of ACL reconstructions.
How does one diagnose a PCL tear on x-rays or MRI?
Diagnosing a PCL tear involves a combination of methods, including stress x-rays, plain x-rays, and MRI scans. The accuracy of these diagnostic tools can vary depending on the timing of the injury.
MRI scans tend to yield excellent results when the PCL tear is acute, indicating that it occurred in the last few weeks. However, in cases where the PCL tear is chronic, the ligament may have a chance to heal, often in a loose position, making it challenging to interpret the extent of the damage on MRI scans. For chronic PCL tears, MRI scans are not as accurate, with an estimated accuracy rate of roughly 60% to 70%.
To ensure a more precise assessment of the PCL tear's severity, especially in both acute and chronic injuries, the use of PCL stress x-rays is recommended. These x-rays provide an objective measurement of instability and serve as a crucial diagnostic tool. Typically, if PCL stress x-rays indicate an abnormal translation of more than 8 mm, it suggests that surgery may be necessary. Therefore, our recommendation for all patients with PCL tears, regardless of the injury's chronicity, is to undergo PCL stress x-rays. This approach allows for an accurate assessment of the injury's extent and informs decisions about the need for surgical intervention.
What are common reasons for PCL reconstruction graft failure?
Graft failure is a significant concern in PCL reconstruction, and one of the most common reasons for graft failure is the improper placement of the graft in a non-anatomic position. When the graft is not positioned correctly, it can lead to gradual stretching of the graft over time. This stretching can compromise the stability and effectiveness of the reconstructed ligament.
Another potential issue that can contribute to graft failure is the reaming of the PCL reconstruction tunnel, which can involve the removal of one of the root attachments. This procedure may inadvertently lead to early-onset arthritis and further contribute to the graft's stretching over time.
To achieve the best possible outcomes in PCL reconstruction surgery, it is crucial to ensure that the graft is placed in an anatomically correct position. This approach helps minimize the risk of graft failure and maintains the long-term stability and function of the reconstructed PCL. Additionally, surgical techniques that preserve the root attachments and prevent the development of arthritis are essential for successful PCL reconstruction outcomes.
When is a brace necessary for PCL reconstructions?
The current gold standard for postoperative care in PCL reconstruction involves the use of dynamic or static PCL braces. These braces play a crucial role in protecting the graft and promoting successful recovery, particularly during the early stages after surgery.
Dynamic PCL braces, in particular, have shown their effectiveness in various studies. These braces are designed to push the tibia forward when the knee bends, which aligns with the natural motion of the knee joint. This proactive movement has been found to enhance the overall success rate of PCL reconstruction procedures.
For patients with acute PCL tears, where the ligament is stressed but not entirely torn, dynamic PCL braces can be especially beneficial. By holding the knee in a reduced position, these braces create an environment that allows the PCL to potentially heal acutely. This approach offers an opportunity for patients to recover and regain knee stability without the need for a full reconstruction.
In summary, the use of dynamic or static PCL braces is a critical component of the rehabilitation process after PCL reconstruction surgery. These braces aid in protecting the graft and facilitating optimal recovery, promoting the best possible outcomes for patients.
What is the return to sport time after a PCL reconstruction?
Understanding the intricacies of a PCL reconstruction surgery is crucial. Unlike some other procedures, PCL reconstruction involves larger grafts, making it essential to implement a slower rehabilitation process. Rushing back to activities before the grafts have had sufficient time to heal can lead to complications, including the stretching of the PCL reconstruction. This risk is particularly relevant in single-bundle PCL reconstructions, especially for patients with a flatter tibial slope.
In general, our primary goal in the recovery process is to ensure that patients achieve a full restoration of their balance, agility, and overall endurance. This comprehensive approach to rehabilitation is aimed at preparing patients for a functional sports test, which typically takes place around 9 to 12 months following the PCL reconstruction. Successful completion of this test is a significant milestone, indicating that the patient is ready to return to their regular activities with confidence.
Ultimately, taking the time for proper healing and a thorough rehabilitation process is key to achieving successful outcomes after PCL reconstruction.
What are the risks of not having a PCL reconstruction with a grade 3 tear?
It's a well-established fact that many athletes can regain their ability to participate in full activities after experiencing a PCL tear. In some cases, they've even managed to extend their careers by 5 to 7 years by opting for nonoperative treatments. However, as we've witnessed the aftermath of numerous such cases, a common trend emerges – over time, the knee often succumbs to wear and tear, leaving patients with a sore and painful knee after 5 to 7 years.
This is where the paradigm shift occurs. Thanks to the evolution of surgical techniques and the revelation that outcomes now rival those of isolated ACL reconstructions, there's a clear consensus among PCL reconstruction surgeons. The current gold standard firmly recommends PCL reconstruction for athletes with these injuries. This approach not only prolongs their careers but also serves as a vital preventive measure against the development of osteoarthritis over time. It's not just about returning to the game; it's about ensuring a healthier, pain-free future for these athletes.
Why choose Kneecares for your PCL Reconstruction
When it comes to young, active individuals who've experienced a complete tear of the PCL, our stance is crystal clear. We strongly advocate for early reconstruction of the ligament to safeguard against the specter of arthritis, which might rear its head in the years to come. Regrettably, many patients who endured a PCL injury in the distant past often find themselves battling arthritis when they finally seek care, sometimes, when it's already too late.
In these cases, the treatment goal typically shifts towards providing pain-free engagement in daily activities, with or without surgery. We've taken strides in developing a highly active rehabilitation program following PCL reconstruction. This program involves immediate knee mobilization and tailored exercises, and the results have been nothing short of remarkable. Our approach has yielded one of the lowest complication rates as documented in the medical literature. For those patients who require surgery, this is undoubtedly heartening news.
It's important to emphasize that the field of PCL surgery is in a state of constant evolution. Newer techniques and refinements emerge every year, further underscoring our commitment to staying at the forefront of advancements in PCL care. Rest assured, we're dedicated to providing our patients with the most effective and innovative treatments available.
