Patellofemoral Pain Syndrome
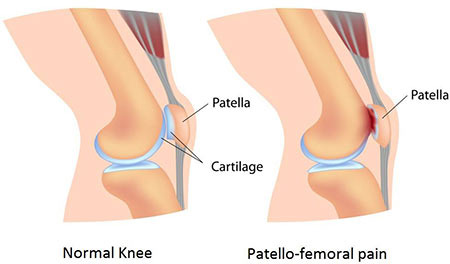
Patellofemoral pain syndrome, also known as chondromalacia patella, runner's knee, or moviegoer's knee, is a condition characterized by discomfort in the patellofemoral joint, which includes the kneecap and the front part of the femur. This condition typically arises from overuse rather than a traumatic injury, and it can manifest during various activities, both athletic and every day.
Patients often notice this pain when:
- Walking up or down stairs
- Transitioning from sitting to standing
- After extended periods of sitting
- Running or engaging in athletic activities
- Squatting, kneeling, or lunging
The discomfort can also be triggered by wearing high heels. While it may be more noticeable during activities that place extra stress on the patellofemoral joint, the pain is generally less pronounced when walking on level ground.
Dr. Amit Meena emphasizes that, upon examination, the pain is frequently located at the lower and outer edges of the kneecap, beneath the patella, and on the outer side of the knee. In cases of heightened inflammation, patients may experience diffuse pain throughout the entire joint.
The syndrome is often associated with an uneven distribution of stress under the kneecap, leading to discomfort. This irregular stress distribution can be attributed to an abnormal tilt of the patella, which is sometimes visible on X-rays. However, it can also occur in individuals with normal X-rays, often due to weakness in the large muscle groups of the leg. When patellofemoral pain sets in, it inhibits the quadriceps muscle, the major muscle in the front of the thigh, from effectively unloading stress on the kneecap. As a result, the pain can progressively worsen.
The syndrome is often associated with an uneven distribution of stress under the kneecap, leading to discomfort. This irregular stress distribution can be attributed to an abnormal tilt of the patella, which is sometimes visible on X-rays. However, it can also occur in individuals with normal X-rays, often due to weakness in the large muscle groups of the leg. When patellofemoral pain sets in, it inhibits the quadriceps muscle, the major muscle in the front of the thigh, from effectively unloading stress on the kneecap. As a result, the pain can progressively worsen.
Patellofemoral pain syndrome, as well as other patellar issues, is more commonly observed in women than in men. Women often adopt a valgus or knock-kneed posture, which naturally pulls the patella toward the outside of the leg, subjecting the knee to uneven stress distribution.
Tight muscles and soft tissues supporting the knee, including the hamstrings and the iliotibial (IT) band, can contribute to this condition. Conversely, women with hypermobile or loose soft tissues can develop the syndrome due to muscle weakness and the inability of supporting muscles to balance or unload the patella, allowing it to be pulled laterally away from the trochlea.
Orthopedic surgeons and sports medicine specialists conduct a comprehensive physical examination to evaluate patellofemoral pain. This assessment includes identifying any imbalances from the feet to the hips. Additional factors that can exacerbate pain include flat feet, abnormal hip rotation, IT band tightness, and issues with hip flexors. In some cases, MRI and X-ray imaging are utilized to assess the bones, alignment, and cartilage surfaces of the kneecap and trochlea, providing a more comprehensive understanding of the condition.
Remember, early diagnosis and appropriate treatment can make a significant difference in managing patellofemoral pain syndrome and enhancing your overall quality of life.
Treatment
Dr. Amit Meena emphasizes that the majority of individuals dealing with patellofemoral pain syndrome can effectively manage their condition without the need for surgery. The initial focus of treatment is to provide relief and "quiet the knee." This is achieved through various non-operative methods.
Anti-inflammatory medications and the application of ice play a crucial role in reducing inflammation and discomfort. It's essential to give your knee some rest and modify activities that exacerbate the condition. This might involve temporarily avoiding high-impact sports, intense workouts, squatting, lunging, and minimizing stair climbing.
In cases where anatomical factors like flat feet are contributing to the issue, orthotics may be recommended. For runners, if landing irregularities, such as pronation or supination, are a part of the problem, a change in footwear may be necessary. Sometimes, a cortisone injection can help reduce knee inflammation, making it more tolerable for the patient to engage in a stretching and strengthening program.
A structured physical therapy regimen is initiated to address tight tissues, enhance structural strength throughout the leg and hip, and promote overall recovery. If the expected improvements aren't achieved through physical therapy, further imaging, such as an MRI with specialized sequences, may be recommended to assess early cartilage changes.
Dr. Amit Meena highlights that a procedure known as a "lateral release" can be beneficial when performed in conjunction with more extensive surgeries like a tibial tubercle osteotomy or a medial patellofemoral ligament (MPLF) reconstruction, as part of a comprehensive soft tissue balancing approach. However, as an isolated procedure, it is suitable for only a very small subset of patients. This includes individuals with a tilted patella, intact cartilage, and a lack of improvement despite extensive physical therapy. It's important to note that more than 95% of patients with patellofemoral pain syndrome do not require surgery.
Managing patellofemoral pain syndrome is often successful through non-operative treatments tailored to the individual's specific condition and needs. Surgery is typically reserved for a select group of patients who have specific, well-defined indications.
